The grieving parents of a young actress who died after being misdiagnosed by a physician’s associate are joining an unprecedented legal action by senior doctors against the General Medical Council.
They say they feel ‘hoodwinked’ by the regulator’s chief executive who, they claim, has reneged on a promise to make sure such tragedies do not happen again.
Marion and Brendan Chesterton’s much-adored daughter Emily, 30, died in 2022 from a clot on the lung which a physician associate (PA) – a healthcare worker with just two years’ training – incorrectly diagnosed as anxiety and a sprain. Amid growing concerns nationally about the use of ‘cut price medics’ to plug staffing shortages, the couple met with General Medical Council boss Charlie Massey in July. He assured them there would be ‘no more Emilys’ when the body begins regulating PAs in December, The Mail on Sunday can reveal.

Emily Chesterton died in 2022 from a clot on the lung which a physician associate incorrectly diagnosed as anxiety and a sprain
The Chestertons left the meeting ‘reassured’ that there would be limits set on what PAs could and could not do.
They believed the GMC would ensure PAs would be properly supervised by qualified doctors – rather than working with little or no oversight, as they all-too-often have been – and required to be clear with patients that they were not doctors.
These points, and particularly the last, were crucial in Emily’s case: she was not told she was seeing a PA – otherwise, her mother Marion says, the family would have sought a doctor’s opinion and they believe she would not have died.
But they now feel ‘let down’ by the General Medical Council after it emerged in legal documents that the regulator has no plans to limit the scope of PAs or anaesthesia associates – and claims it has ‘no power’ to do so.
The documents, seen by this newspaper, have emerged as part of a judicial review being launched by campaign group Anaesthetists United.
They also suggest the regulator will not require associates to outline their ‘skills and experience’ to patients, nor will it define how they should be supervised.
The revelations have led the Chestertons – and other grieving families whose loved ones have fallen victim to PA errors – to join in the Anaesthetists United legal action. Their aim is to force the council to clearly define the limits of PA roles to stop them performing doctors’ tasks. The NHS plans to recruit 10,000 physician and anaesthesia associates – abbreviated to AAs – by 2038 to relieve strain on the service.
But over the past year, The Mail on Sunday has uncovered repeated incidents of PAs overstepping their intended role: for basic tasks such as filling in forms and performing basic health checks to free up doctors’ time.
We have uncovered evidence of PAs diagnosing patients, carrying out operations, prescribing drugs and covering doctors’ shifts.
As part of our campaign to Rein In The Physician Associates we have also reported a number of deaths and even a baby left disabled due to PA blunders.
Doctors are also concerned. On Friday, the Royal College of GPs voted overwhelmingly to ban PAs from working in GP surgeries.
Speaking to the MoS, retired languages teacher Mrs Chesterton said: ‘During our meeting, Mr Massey agreed with more or less everything I said we wanted to achieve and the fact that patient safety should be paramount.
‘At the end, he looked at me and said: “I promise you, no more Emilys”. We came away very reassured that the kind of regulation we wanted would be in place.
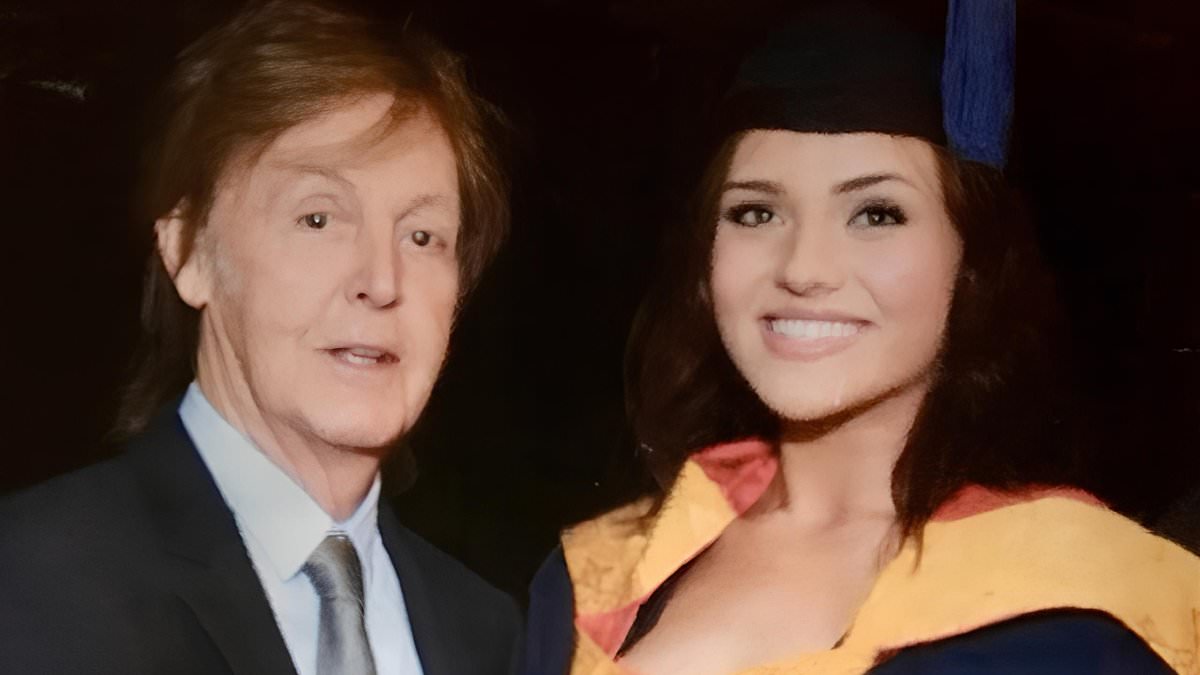
‘I even sent him a photo of Emily afterwards, asking him to keep her at the forefront of his mind when he was planning how regulation would go. It was one of her with Paul McCartney, taken at her 2017 graduation from the Liverpool Institute of Performing Arts – she was beaming and we were so proud of her.
‘But now, having seen from legal letters that proper regulation isn’t going to be sorted, I wonder whether we were being a bit placated, a bit hoodwinked.
‘We’re getting involved in the legal action to prevent any other families going through the same hell. The General Medical Council need to live up to their responsibilities. We need absolute clarity on what PAs and AAs can and cannot do.’ In a letter sent by the General Medical Council to lawyers representing Anaesthetists United in August, the regulator insists the Government does not require it to limit PAs’ tasks – just set ‘standards’ for their training and skills. It says the Department of Health could have ordered the regulator to impose such limits, ‘however it chose not to’.

Emily beaming in a photo with Paul McCartney, taken at her 2017 graduation from the Liverpool Institute of Performing Arts
In addition, while the General Medical Council’s website says PAs should have ‘some degree of supervision’ this should be determined by employers – in other words, hospital trusts or GP surgeries. The letter also says ‘there is no requirement’ for associates ‘to inform patients of their experience or qualifications before treating them’ – although the regulator has insisted to the MoS they would still be required to introduce themselves to patients and explain their role.
Mrs Chesterton said the tone of the letter ‘is completely different to her meeting with Mr Massey. ‘It’s so arrogant and passing down responsibility yet again. ‘Families who’ve lost loved ones don’t care about the distinction between standards or limits, we just want to know that regulation will be robust.’ The letter adds that medical Royal Colleges would be the ‘appropriate bodies’ to provide guidance on their scope of practice.
However, Royal Colleges have no regulatory powers – and the General Medical Council has not said if it will enforce any guidance they produce.
Solicitor John Halford from Bindmans, acting for Anaesthetists United, said: ‘Guidance from Royal Colleges has no teeth. Without clear limits from the General Medical Council, AAs and PAs can do what they believe they’re capable of, or what their Trust tells them to do.
‘There is no limit – that’s the sort of Wild West we have at the moment and what led to Emily Chesterton’s death. It’s a regulatory cop-out.’ Evidence suggests existing guidance from the Royal College of Anaesthetists on the use of AAs – with updated draft guidance due soon – is already being flouted by hospitals and is open to interpretation.
Documents retrieved by Anaesthetists United under Freedom of Information laws reveal ‘really quite shocking’ policies at a local level, according to Mr Halford.
They show AAs are being allowed to sedate patients, including children, without direct supervision from a doctor. In some cases, supervising doctors don’t have to be in the same room or hospital building – but should be able to get there within a few minutes. Others say doctors just need to be contactable by phone.
In some cases, AAs are being allowed to decide what drugs to give patients.
In a recent study of patients who suffered a cardiac arrest during surgery, 47 per cent died when an AA was in charge of their anaesthesia, which fell to 30 per cent if they were not.
As for PAs’ scope, there is no guidance at all by the Royal College of Physicians. It is embroiled in a separate controversy, accused of ‘deliberately misleading Parliament’ by suggesting in a Government consultation its members were in favour of the General Medical Council regulating PAs. In fact, many object to it overseeing PAs as it further blurs the lines between PAs and doctors.
Doctors wrote an open letter to the British Medical Journal (BMJ) last week condemning the RCP leadership.
Further FoI documents reveal the General Medical Council was paid £8.1million over three years by the Department of Health to put together the regulation package, with a further pay-out of £2.2million anticipated as being necessary by this year.
Dr David Nicholl, a neurologist in Birmingham and one of the signatories of the letter sent to the BMJ, said this indicated the regulator was ‘acting as an arm of government rather than putting patient safety first’.
Another case included in the legal action is that of Susan Pollitt, who died last year following an unnecessary medical procedure carried out by a PA.

Emily graduating in 2017. Concerns are growing nationally about the use of ‘cut price medics’ to plug staffing shortages

Emily, front right, as a young girl with her mother Marion, father Brendan and sister Jasmine
Susan, 77, went to the Royal Oldham Hospital in Greater Manchester after falling and breaking her arm in July 2023. She died of a bacterial infection from the procedure.
Coroner Joanne Kearsley said there was ‘no adequate procedure’ for ensuring PAs were capable of carrying out such operations at the Northern Care Alliance, which runs the hospital. She took the unusual step of writing to the General Medical Council and now Health Secretary Wes Streeting, warning of a risk of further deaths unless action was taken to better regulate PAs.
A General Medical Council spokesman said: ‘We have been consistent in saying that we will expect PAs and AAs to always work under some degree of supervisionand to practise within their competence. They will have a responsibility to clearly communicate who they are and their role in the team.
‘To register with us, PAs and AAs will also need to show that they have the knowledge, skills, and experience to treat patients safely, and that there are no outstanding concerns about their fitness to practise.
‘Bringing PAs and AAs into regulation will help to assure patients, colleagues and employers that they are safe to practise and can be held to account if serious concerns are raised.’
- Anaesthetists United needs to raise £200,000 by the end of the month to fund its legal case against the General Medical Council. Donate here: crowdjustice.com/case/stop-misleading-patients