Disorders Cure
oi-Shivangi Karn
on June 11, 2021
As India’s deadly second wave of COVID-19 has peaked, the post-complications in recovered patients have risen drastically, starting from the fatal black fungus or mucormycosis, followed by a white fungus, yellow fungus, blood clots, gangrene, COVID nails and now, herpes simplex virus infection.
According to recent news reports, a hospital in Ghaziabad located a few kilometres from Delhi, has reported the first case of herpes simplex virus infection, which is even called “very dangerous” according to doctors of the hospital. The herpes virus was found in the nose of the patient.
The report adds that people who have recovered from COVID-19 and have a weakened immune system or still suffering from the condition are at increased risk of herpes simplex virus.
What Is Kala-Azar (Black Fever)? Causes, Symptoms, Risk Factors, Treatments And Prevention
The herpes infection can be deadly when there’s a delay in treatment. The increased cost of the treatment could be the main cause for delaying the treatment, making the virus deadlier than COVID-19.
In this article, we will discuss the herpes simplex virus and its association with COVID-19. Take a look.

What Is Herpes Simplex Virus Infection And Its Risk Factors ?
Herpes simplex virus (HSV) is a virus type that is known to cause an infection called herpes or herpes simplex virus infection. It is among the most contagious and frequently encountered infections in humans.
A study says that out of more than 80 herpesviruses, eight are known to affect humans and cause serious complications, especially in immunocompromised individuals. [1]
There are two types of herpes simplex virus: Herpes simplex virus type 1 (HSV-1) and Herpes simplex virus type 2 (HSV-2).
- HSV-1: Major risk factors for HSV-1 include exposure to infected person’s saliva such as by sharing drinking water, cosmetics or mouth to mouth contact. Other risk factors include sharing of razors, nail-biting (especially in children), immunocompromised states (especially for severe or chronic HSV). [2]
- HSV-2: Major risk factors for HSV-2 include direct exposure to infected fluids, especially during sexual intercourse. HSV-2 has low stability outside the body, therefore, it can only remain infectious for days in moist environments or surfaces like bodily fluids that include saliva and vaginal fluid. [3] The infection, if present in pregnant women, can be transferred to intrauterine and cause congenital HSV infection.
- Genital-to-genital contact such as sexual intercourse without protection. [4]
- Oral-to-oral contact such as kissing, touching the mouth sores or surfaces around the mouth.
- Oral-to-genital contact. [5]
- Sharing razors, lip balms or dishes
- Sharing sex toys
- Having any other genital or oral contact with the infected person.
Yoghurt For Diabetes: Is It A Healthy Option?
Causes Of Herpes Simplex Virus Infection
As aforementioned, the herpes virus is contagious and can easily pass on from one person to another through skin-to-skin contact or direct contact with the mucous membranes such as the mouth, eyes, genitals and anus, where the virus is in high infectious form.
The infection cannot be caused when a person touches the infected object or surfaces such as a towel or washbasin. Directly touching a herpes sore can infect an individual. Even in the absence of sores, a person can spread the virus. This is called “asymptomatic viral shedding.”
Some of the ways in which an infected person can pass the virus are:
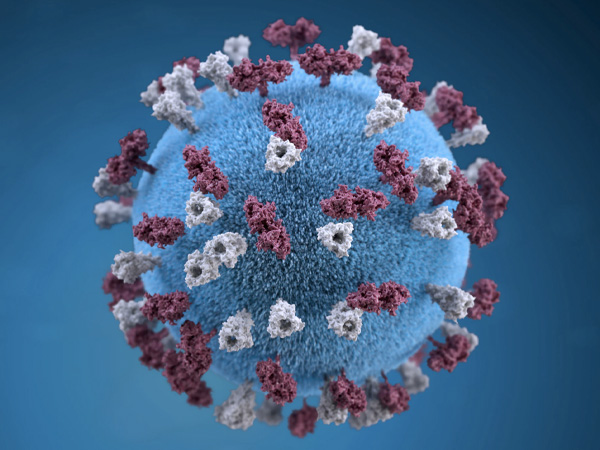
COVID-19 And Herpes Simplex Virus Infection
Though the first case of COVID-related herpes has been reported recently in India, it’s not the first case reported globally.
Earlier, a study published on 9 January 2021 talks about the same condition in a 69-year-old Caucasian male. [6]
The patient has a medical history of coronary artery disease, type 2 diabetes mellitus, stage III squamous cell lung cancer and peripheral arterial disease.
Along with dyspnea, he also reported bilateral eye pain with the development of an eyelid ulcer. Samples from eye secretions showed positive for HSV-1 conjunctivitis (HSV that has spread to the eyes) and negative for COVID-19.
READ RELATED: Three DIFFERENT daily coronavirus death tolls ‘to be published after Public Health England exaggerated numbers’
The COVID-19 was managed with hydroxychloroquine and HSV-1 in the eyes was treated with famciclovir, along with many other supportive cares and therapies.
COVID Nails: Is It A Serious Sign Related To COVID-19?
Symptoms Of Herpes Simplex Virus Infection

Who Is At Increased Risk Of Herpes?
- Females, as herpes commonly arises on the vagina and vulva due to their mucosity. [7]
- In males, herpes are found in the foreskin or top of the penis. It is common in homosexual males. [8]
- People with multiple sex partners.
- People with a weak immune system.
- People who have sex at a younger age.
- People having another sexually transmitted disease such as hepatitis.
- Minor surgery
- Emotional stress
- Any illness that can weaken your immune system
- High fever
- Hormonal fluctuations such as menstrual periods
- Sun exposure
Mixing And Matching Of COVID-19 Vaccine Doses? Is It Safe?
What Is Recurrent Herpes Simplex And Why It Is Considered Dangerous?
Once the herpes virus initially infects a person, be it HSV-1 or HSV-2 or whether a person is symptomatic or not, the virus never leaves the body of the person, especially in people with HSV-2 infection. [10]
After initial infection, the virus moves to the nerve cells from the skin cells and stays there forever in the dormant state, until they become active again due to certain triggering factors.
Some of the triggering factors include:
Note: In some cases, there is no particular cause for eruption. Recurrent simplex herpes gets triggered on the same site as the primary infection such as lips and genitals.

Complications Of Herpes Simplex Virus Infection
If not treated early, herpes can cause complications such as:
- HIV, especially when the infection is severe and recurrent.
- Encephalitis or inflammation of the brain. [11]
- Keratitis or inflammation of the cornea.
- Tender swollen lymph nodes in the genitals.
- Severe ulceration of the cervix. [12]
- Serious neurologic disability in newborns if transferred from pregnant woman to child.
- Decrease in the quality of life and sexual relationships.
- Physical examination: To look out for herpes sores.
- Herpes culture: It is recommended after herpes sores are identified. The fluid from the sores is taken for examination of the herpes virus. [13]
- Blood tests: To look for antibodies of HSV-1 or HSV-2.
- MRI: If a medical expert suspects transmission of the virus to the brain.
- Prescribed antiviral medications: Such as acyclovir, valaciclovir, and famciclovir to promote healing of the sores and decrease the probability of excreting the virus. [14]
- Antiviral cream or ointments: To get relief from itching, burning or tingling.
Note: Serious complications of herpes rarely occur in healthy adults. Newborns, people with weak immune systems, people with long-term illness or people who have had surgery or organ transplant are more prone to getting affected by the virus.
Women With Advanced HIV Carried COVID-19 Virus For 216 Days, Says New Study
Diagnosis Of Herpes Simplex Virus Infection?
Some of the diagnostic methods for herpes include:
Treatment Of Herpes Simplex Virus Infection
There is no cure for herpes simplex virus infection. Only the sores or other physical symptoms of the infection could be treated. Some of the treatment methods for herpes include:

Prevention Of Herpes Simplex Virus Infection
As there is no cure for herpes, it can only be prevented by avoiding the transmission of the virus. If you are experiencing HSV-1, take preventive measures like:[15]
- Avoiding skin-to-skin contact with other people.
- Avoiding kissing, oral sex or any type of sexual activity.
- Avoid sharing objects like towels, utensils, drinking bottles, cosmetics or clothes.
- Maintain hand hygiene and avoid touching sores.
- Use sunscreen if you have an oral HSV infection or avoid sun exposure at all.
- Use condoms during sexual intercourse. However, experts suggest avoiding sex at all as the virus can still pass to your partner from uncovered skin.
- If you are pregnant and observe triggering of HSV, consult a medical expert soon for medications to prevent the transmission of the virus to the unborn child
- Avoid conditions that can trigger the HSV.
To Conclude
COVID-19 tends to weaken the immune system in some recovered patients and make them prone to other infections or diseases. Although the prevalence of herpes simplex is not high in India, with the advent of the COVID-19, the cases of COVID-related herpes can increase among COVID recovered patients due to their weakened immunity.
Doctors advise recovered patients to remain cautious post hospitalisation and take good care of their health.
GET THE BEST BOLDSKY STORIES!
Allow Notifications
You have already subscribed
Source:








