Get to know “Is Celiac Disease Genetic Or Hereditary?” Encountering this article suggests that either you or someone within your circle is grappling with celiac disease.
My personal journey involves a diagnosis of celiac disease over a decade ago, leading me to amass a profound understanding of this condition.
Drawing upon my extensive experience and expertise as a celiac disease patient, I am distinctly positioned to aid you in comprehending and effectively managing this consequential disorder.
What is Celiac Disease?
Celiac disease is a genetic autoimmune disease that affects about 1 in 100 people, which is about one percent of the population.
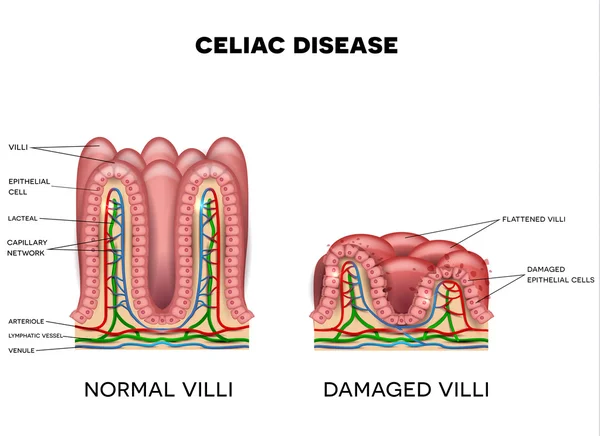
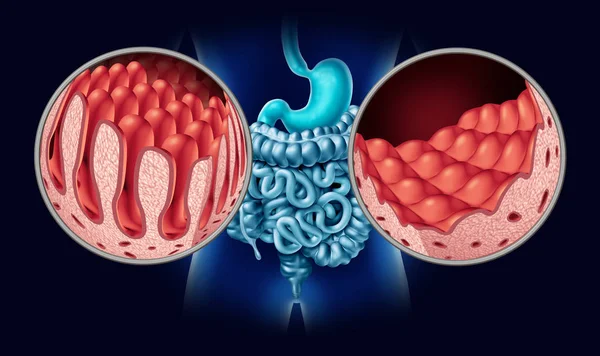
When someone has celiac disease, their immune system becomes confused and mistakenly attacks the healthy tissue surrounding the small intestine whenever they eat gluten, a protein found in wheat, rye, barley, and sometimes oats.
The attack is swift and constant. Over time, the person’s microvilli, or the hair-like follicles surrounding the small intestine, become damaged and flattened. This is known as villous atrophy.

What most people don’t realize is that the small intestine is a vital organ that feeds every other organ and cell in the body. In other words, without a properly functioning small intestine, a person can become malnourished and nutrient deprived, all of which can lead to various disorders throughout the body.
There are dozens of symptoms related to celiac disease beyond the classical gastrointestinal symptoms (bloating, gas, diarrhea, etc.) that most people associate with the disease. These symptoms include but are not limited to the following:
- Nutrient deficiencies (anemia, Vitamin B deficiency, feeling shaky between meals)
- Osteopenia or osteoporosis
- Fatigue
- Joint pain or arthritis
- Weight loss
- Diarrhea
- Constipation
- Bloating
- Chronic gas
- Failure to thrive and short stature (children)
- Dental (enamel) issues
- Irregular menstruation
- Fertility issues
- Depression, anxiety, or other mental and/or behavioral disorders
- Dermatitis herpetiformis (also known as celiac rash)
- Hair loss
- Oral issues (canker sores, geographic tongue)
Some people experience what is known as silent celiac disease, which means they have no blatant celiac symptoms, yet they have an autoimmune disorder.
Is Celiac Disease Genetic Or Hereditary? According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), celiac disease is a genetic disorder that runs in families. People with a first-degree relative (parent, sibling, or child) with celiac disease have a 10% chance of developing the disease themselves. Celiac disease is caused by certain genes that are passed down from parents to their children. However, not everyone who inherits the genes for celiac disease will develop the disease. In fact, only about 1 in 100 people who carry the genes will ever develop symptoms. Here are some additional expert opinions on celiac disease and its genetic basis: Dr. Alessio Fasano, MD, Director of the Celiac Disease Center at the University of Maryland School of Medicine: "Celiac disease is a complex genetic disorder that is caused by a combination of genetic and environmental factors. The genes that are most strongly associated with celiac disease are HLA-DQ2 and HLA-DQ8, but not everyone who carries these genes will develop the disease. There are also a number of environmental factors that can trigger celiac disease, such as certain viral infections or exposure to gluten at an early age." Dr. Joseph Murray, MD, Professor of Medicine at the Mayo Clinic: "Celiac disease is an autoimmune disorder that is caused by a reaction to gluten, a protein found in wheat, rye, and barley. People with celiac disease have a genetic predisposition to the disease, but environmental factors also play a role. For example, people who have a family history of celiac disease are more likely to develop the disease if they start eating gluten at an early age." Dr. Peter Green, MD, Professor of Medicine at Columbia University: "Celiac disease is a serious but manageable condition. With a strict gluten-free diet, most people with celiac disease can live long and healthy lives. It is important to diagnose celiac disease early, as untreated celiac disease can lead to a number of complications, such as osteoporosis, anemia, and infertility." If you are concerned that you or someone you know may have celiac disease, it is important to talk to your doctor. They can order blood tests to check for celiac disease antibodies and recommend a biopsy of the small intestine to confirm the diagnosis.
Testing and Diagnosing Celiac Disease
Celiac disease can be diagnosed (by a doctor) using a simple blood test. Many people will take an at-home celiac disease screening test (pictured below), then discuss the results with their doctor.
If the test is positive, they likely have celiac disease, and many physicians will follow up the blood test with an endoscopy procedure to biopsy and examine the small intestine.
If a blood test is negative, but a person suspects they have an issue with gluten, a doctor might recommend that they go on an elimination diet to see if they’re gluten intolerant instead.
My blood test was positive for celiac disease. I then visited a GI doctor who biopsied my small intestine and confirmed celiac disease. This is the gold standard method for testing for and diagnosing celiac disease.
Is Celiac Disease Genetic?
Celiac disease is a genetic disorder, and people with celiac disease carry either or both the HLA-DQ2 or HLA-DQ8 genes.
Research shows that people with a first-degree relative with celiac have a higher risk of getting the disease, and siblings of first-degree relatives have the greatest genetic risk.
You can undergo genetic testing to determine if you carry one of the celiac disease genes. You can also take this at-home genetic test (pictured below) to see if you carry one of the two celiac genes.
Celiac disease can turn on at any time in genetically predisposed people. This means someone with one of the celiac genes might test negative for celiac disease one day and, years later, test positive. Genetic screening can help determine whether annual celiac disease screening is necessary.
I tested both of my kids for the celiac gene. My son doesn’t carry either gene, but my daughter carries one of the genes (the same one I carry). This means I will need to screen my daughter for celiac annually, but not my son.
Just because someone has one of the celiac genes does not mean they have or will get celiac disease, gluten intolerance is a precursor to celiac disease in genetically predisposed people.
What Causes Celiac Disease?
While you must have a genetic predisposition to celiac disease to have the disorder, researchers have found that two additional factors must also be present.
First, you must also be eating gluten (obviously), and second, you must experience some intestinal permeability (leaky gut), which is often triggered by poor eating habits, viruses, trauma, antibiotics, or a weakened immune system.
When someone with celiac stops eating gluten, their symptoms resolve with some exceptions, like those with non-responsive refractory celiac disease.
In many people, celiac disease develops over time, with gluten slowly damaging the small intestine like a leaky faucet. Eventually, after years of eating gluten, the pipe bursts, and poof, a person has full-blown celiac disease.
Testing for Celiac Disease
Getting tested for celiac disease requires a simple blood test that can be performed by a doctor or discreetly at home using this celiac disease screening test.
If the test is positive, a doctor may want to perform an endoscopy procedure to biopsy the small intestine and look for damage consistent with celiac (flattened villi and inflamed small intestine lining).
If the blood test is negative, the doctor might want to evaluate a person for non-celiac gluten sensitivity, perform a celiac disease genetic test, or look for other related disorders like acid reflux, IBS, Crohn’s, SIBO, candida, etc.
I suggest reading 15 Foods That Cause Digestive Problems. Most experts say if you suspect you have an issue with gluten, you should do an elimination diet for 4-6 weeks.
Managing Celiac Disease
I can attest that managing celiac disease is a bear and something a person can never take a break from doing. Currently, the only treatment option for celiac disease is a strict gluten-free diet.
READ RELATED: Sam’s Club Is Offering Crazy Cheap Membership Fees For a Limited Time
Despite not being able to eat gluten, people with celiac disease can still enjoy a variety of naturally gluten-free foods, including fresh fruits and vegetables, cheeses, meats, fish, eggs, beans, potatoes, lentils, and various gluten-free grains, including rice, buckwheat, and quinoa, as well as these 9 Foods You Can Eat on the Gluten-Free Diet.
While a whole foods diet is best for those with celiac disease, it’s not always easy to do, and many people want to enjoy packaged foods or eat at restaurants from time to time.
Unfortunately, gluten is found in many confusing ingredient labels and hidden foods, like soy sauce and licorice. This is why label reading is one of the most important skills a person with celiac disease can master.
Many restaurants don’t understand the ins and outs of creating a safe, gluten-free meal free and that even a crumb of gluten can hurt their gluten-free customers. This is why learning to eat out safely is top of mind for many people with celiac disease.
Long-Term Prognosis for Celiac Patients
For those following a gluten-free diet and properly managing their symptoms, the prognosis is good.
Many people (including me) have put their celiac disease symptoms into remission by adhering to a strict gluten-free diet. While the disease will never go away, it can become dormant.
However, many individuals struggle to fully adhere to a gluten-free diet, especially since gluten is addictive.
Dr. William Davis, in his New York Times best-selling book, Wheat Belly, talks about gluten’s opiate-like effect on the brain. He says wheat is hard to give up and causes distinct withdrawal symptoms in those who stop eating it. While the gluten-free diet is the only treatment option for people with celiac disease, it also is a difficult treatment regimen for many to follow.
On top of that, some people suffer from gluten cross-contamination or occasionally get accidentally glutened. Some don’t take their disorder seriously and choose to cheat on their gluten-free diet.
Unmanaged (or improperly managed) celiac disease can lead to additional autoimmune diseases, fertility issues, worsening and painful symptoms, and serious, life-threatening diseases such as cancer, particularly intestinal lymphoma and small bowel cancer. Commonsense says anyone living in a chronic state of inflammation is ripe for disease.
A study published in Gastroenterology said that the later in life someone is diagnosed with celiac, the higher their risk of getting additional autoimmune diseases.
Living with Celiac Disease
Celiac disease is a lifelong affliction that must be continually managed via a strict, gluten-free diet. Currently, there is no cure for celiac.
As someone who lives with celiac daily, I uniquely understand the challenges. The daily struggle and emotional burden of the gluten-free diet are real. It’s not easy to eat out, travel, shop for groceries, or eat at a friend’s house. You must always find ways to balance dietary vigilance with the day-to-day realities of life.
Eating with friends and family is the fabric of Western culture. Most social plans revolve around food. I’ve spent many years figuring out ways to mitigate the risks of eating out and getting sick from accidental gluten exposure.
I also occasionally use a Nima Sensor, the portable gluten-detecting device pictured below, to help me eat out safely and decode packaged foods for hidden gluten. Please read my article, What Not to Eat After Rhinoplasty (Nose Job): A Comprehensive Guide

I believe you can live a healthy, happy life with celiac, but you must always be vigilant and aware of everything you eat. Labeling reading, advocating for yourself, and communicating the seriousness of your diet can help you mitigate the risks of accidentally eating gluten.
Celiac disease has a high treatment burden that requires a person to overhaul and restrict their diet. And while many people with celiac disease agree that it’s nice not to have to depend on pharmaceutical companies to help manage their disease, the burden of the gluten-free diet weighs heavily on the community.
FAQs
Is celiac disease genetic?
Yes, celiac disease is a genetic disorder that runs in families. People with a first-degree relative (parent, sibling, or child) with celiac disease have a 10% chance of developing the disease themselves. The risk of developing celiac disease decreases with each generation. For example, second-degree relatives (aunts, uncles, grandparents) have a 2.5% chance of developing the disease.
What genes are associated with celiac disease?
The most strongly associated genes with celiac disease are HLA-DQ2 and HLA-DQ8. These genes are part of the human leukocyte antigen (HLA) complex, which is responsible for helping the immune system recognize and fight off infections. In people with celiac disease, the HLA-DQ2 and HLA-DQ8 genes make the immune system more likely to react to gluten, a protein found in wheat, rye, and barley.
Does having the HLA-DQ2 or HLA-DQ8 genes mean I will definitely develop celiac disease?
No, having the HLA-DQ2 or HLA-DQ8 genes does not mean you will definitely develop celiac disease. In fact, only about 1 in 100 people who carry the genes will ever develop symptoms. There are other genetic and environmental factors that play a role in whether or not someone develops celiac disease.
What are the environmental factors that can trigger celiac disease?
Some potential environmental triggers for celiac disease include:
- Exposure to gluten at an early age: Infants who are introduced to gluten before 6 months of age are at increased risk of developing celiac disease.
- Certain viral infections: Viral infections have been linked to the development of celiac disease in some people.
- Emotional stress: Emotional stress can trigger celiac disease in people who are already genetically predisposed to the disease.
How can I prevent celiac disease?
There is no way to prevent celiac disease if you have the genetic predisposition for it. However, you can reduce your risk of developing symptoms by following a strict gluten-free diet. A gluten-free diet is essential for managing celiac disease and preventing complications.
Should I get tested for celiac disease if I have a family history of the disease?
Yes, you should get tested for celiac disease if you have a family history of the disease. Early diagnosis and treatment of celiac disease can help prevent complications and improve your overall health.
Note: This article is written based on scientific evidence found by the 247newsaroundtheworld.com team. Sources are duly referenced with keywords hyperlinked to source websites and are clickable for reference.









