Rheumatoid arthritis (RA) Symptoms is becoming more common. A recent global study published in Lancet Rheumatology predicts that the number of RA cases will increase by over 80 percent in the next 26 years. Notably, women are two to three times more likely to develop RA than men, suggesting they will bear a significant part of this rise. The first step in managing the condition is to recognize the early symptoms of rheumatoid arthritis that signal a problem.
While RA can affect anyone, its symptoms typically appear between the ages of 60 and 70. Although there is no cure for RA at this time, recent advancements have made it a more manageable condition. People are much more likely to achieve remission if they consult a specialist early on. Here are the key points to keep in mind.

What Is Rheumatoid Arthritis?
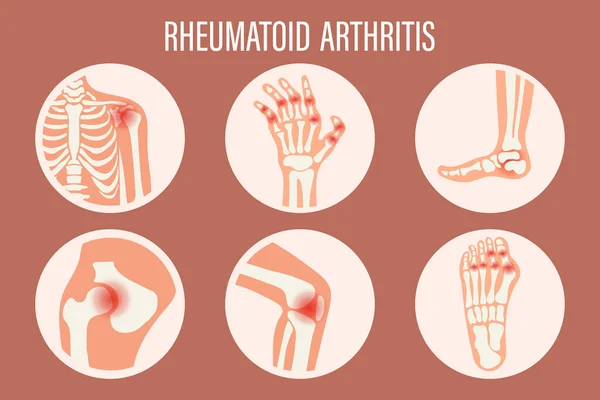
Imagine your immune system mistakenly declaring war on your joints. That’s essentially what happens in rheumatoid arthritis. The immune system attacks the synovium, the lining of the joints, leading to inflammation, pain, and progressive damage. Unlike osteoarthritis, which is a result of wear and tear, RA is systemic and can affect other parts of the body, including the eyes, lungs, and heart.
Dr. Adewale Adebajo, a consultant rheumatologist at Barnsley Hospital NHS Foundation Trust, puts it succinctly: “RA is a condition where the immune system goes awry, targeting healthy joint tissues as if they were harmful invaders. This triggers chronic inflammation that can impact not just the joints but also other organs.” Dr. Adebajo emphasizes that early diagnosis is crucial for effective management.
Common Rheumatoid Arthritis Symptoms
RA can develop gradually or suddenly. Recognizing early symptoms can significantly improve treatment outcomes. Here are some key signs to watch out for:
Joint Pain and Stiffness
- The pain often feels like a throbbing ache.
- Stiffness is typically worse in the morning or after periods of inactivity and can last longer than 30 minutes.
Swelling and Warmth
- Inflamed joints may become swollen, tender to touch, and warm.
Symmetrical Joint Involvement
- RA often affects the same joints on both sides of the body, like both wrists or both knees.
Fatigue and General Symptoms
- People with RA often feel extremely tired or feverish.
- Weight loss and loss of appetite are also common due to systemic inflammation.
Other Signs
- Rheumatoid nodules (firm lumps under the skin near affected joints).
- Symptoms in other areas, such as dry eyes or chest pain, if organs are involved.
If these symptoms persist for weeks, it’s essential to consult a healthcare provider promptly.
Is Rheumatoid Arthritis Genetic?
While RA isn’t directly inherited, genetics play a significant role in increasing susceptibility. Having a first-degree relative with RA can raise your risk by two to five times. Specific genes like HLA-DRB1, STAT4, and PTPN22 are linked to a higher risk of developing RA.
However, genetics isn’t the only factor. Environmental triggers such as smoking, obesity, infections, or hormonal changes also contribute significantly to disease onset. For example, smoking doubles the risk of RA in genetically predisposed individuals, and women are more likely to develop RA than men due to hormonal influences.
Does Cracking Your Knuckles Cause Arthritis?
There’s a common myth that cracking your knuckles leads to arthritis. Dr. John Fackler from Houston Methodist Hospital reassures us: “There are no known detrimental effects to cracking your knuckles.” The sound comes from gas bubbles bursting in joint fluid—not from joint damage. So, while it might annoy those around you, rest assured it won’t cause arthritis.
How Is Rheumatoid Arthritis Treated?
Managing RA involves reducing inflammation, alleviating symptoms, and preventing joint damage. Treatment typically includes:
Medications
- Disease-Modifying Anti-Rheumatic Drugs (DMARDs): These slow disease progression by targeting immune responses. Methotrexate is often the first-line treatment.
- Biologic Agents: Target specific inflammatory pathways (e.g., TNF inhibitors).
- Corticosteroids: Provide short-term relief for acute flares.
- NSAIDs: Help manage pain and inflammation.
Lifestyle Changes
- Regular low-impact exercises like swimming improve joint flexibility.
- Anti-inflammatory diets rich in omega-3 fatty acids (e.g., salmon) may help reduce symptoms.
- Avoid smoking and maintain a healthy weight to lower inflammation levels.
Physical Therapy
- Physical therapy helps strengthen muscles around affected joints while improving mobility.
Surgery
- In severe cases where joint damage is extensive, surgical options like joint replacement may be considered.
Spotting RA Early: A Key to Better Outcomes
Early diagnosis of RA allows for timely intervention with DMARDs or biologics, which can prevent irreversible joint damage. If you experience persistent joint pain or stiffness lasting more than six weeks—especially if it’s symmetrical—don’t delay seeking medical advice.
Living Well with RA
While there’s no cure for rheumatoid arthritis yet, advancements in treatment have made it possible for people with RA to lead fulfilling lives. By staying informed about early symptoms and treatment options—and working closely with healthcare providers—you can manage your condition effectively.
If you suspect you have RA or have concerns about your risk factors, consulting a rheumatologist can provide personalized guidance tailored to your needs.
Also Read | Mini Stroke: Causes, Symptoms, and Prevention Tips








