Let’s look at Understanding Atrial Fibrillation – Atrial fibrillation (AFib) is the most common type of arrhythmia or irregular heartbeat. It occurs when the upper chambers of the heart (the atria) beat too fast and irregularly. This can cause blood to pool in the atria, increasing the risk of blood clots forming. If a blood clot dislodges and travels to the brain, it can cause a stroke.
Types of atrial fibrillation
There are three main types of atrial fibrillation:
- Paroxysmal AFib: This type of AFib comes and goes on its own, and episodes typically last less than seven days.
- Persistent AFib: This type of AFib is continuous and does not go away on its own.
- Long-standing persistent AFib: This type of AFib is persistent and has been present for more than one year.
Causes of Atrial fibrillation
The exact cause of atrial fibrillation is not always known, but it is thought to be caused by a combination of factors, including:
- Structural heart disease: This can include conditions such as coronary artery disease, heart failure, and valvular heart disease.
- Non-structural heart disease: This can include conditions such as hyperthyroidism, pulmonary embolism, and sleep apnea.
- Other risk factors: These include age, family history, high blood pressure, diabetes, obesity, excessive alcohol consumption, and smoking.
Risk factors of atrial fibrillation
The following are some of the risk factors for atrial fibrillation:
- Age: The risk of atrial fibrillation increases with age.
- Family history: If you have a family history of atrial fibrillation, you are more likely to develop the condition yourself.
- High blood pressure: High blood pressure can damage the heart and increase the risk of atrial fibrillation.
- Diabetes: Diabetes can damage the heart and increase the risk of atrial fibrillation.
- Obesity: Obesity can increase the risk of atrial fibrillation.
- Excessive alcohol consumption: Excessive alcohol consumption can damage the heart and increase the risk of atrial fibrillation.
- Smoking: Smoking can damage the heart and increase the risk of atrial fibrillation.
- Other medical conditions: Other medical conditions, such as hyperthyroidism, pulmonary embolism, and sleep apnea, can also increase the risk of atrial fibrillation.
Symptoms of Atrial Fibrillation
Common symptoms of atrial fibrillation:
- Heart palpitations. These feel like a fast, fluttering, or pounding heartbeat.
- Shortness of breath.
- Lightheadedness.
- Fatigue.
- Dizziness.
- Reduced ability to exercise.
Less common symptoms of atrial fibrillation:
- Chest pain.
- Weakness.
- Confusion.
- Fainting.
Some people with atrial fibrillation have no symptoms at all. Their condition may only be detected during a routine physical examination.
If you experience any of the symptoms of atrial fibrillation, it is important to see a doctor right away. Atrial fibrillation is a serious medical condition, but it can be treated effectively with medication or other procedures.
Emergency symptoms
If you experience any of the following symptoms, call 911 immediately:
- Chest pain that is sudden, severe, or spreads to your arms, back, neck, or jaw.
- Shortness of breath that is severe or occurs at rest.
- Fainting.
These symptoms may be signs of a heart attack or stroke, which are both serious medical emergencies.
Diagnosis of atrial fibrillation
Physical examination
During a physical examination, your doctor will listen to your heart and check your pulse. They may also ask you questions about your symptoms and medical history.
Electrocardiogram (EKG)
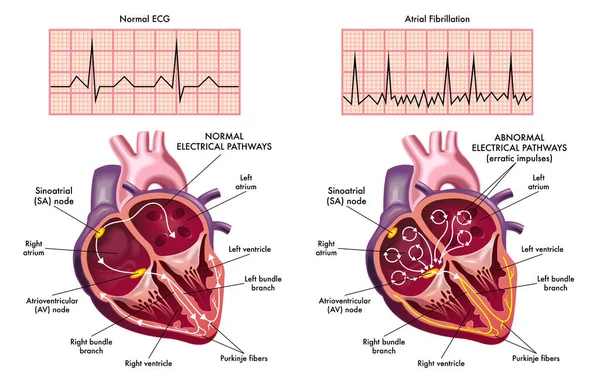
An EKG is the main test used to diagnose atrial fibrillation. It measures the electrical activity of your heart. During an EKG, sticky patches called electrodes are placed on your chest, arms, and legs. The electrodes are connected to a machine that records your heart’s electrical signals.
An EKG can show the rhythm of your heartbeat and how fast or slow your heart is beating. It can also show if you have atrial fibrillation or other heart problems.
Other tests
If your doctor suspects that you have atrial fibrillation, they may order additional tests, such as:
- Blood tests. Blood tests can check for thyroid problems, electrolyte imbalances, and other conditions that can cause atrial fibrillation.
- Echocardiogram. An echocardiogram is an ultrasound of your heart. It can show the structure and function of your heart, including the size and pumping power of your heart chambers.
- Holter monitor. A Holter monitor is a portable EKG device that you wear for 24 to 48 hours. It records your heart’s electrical activity while you go about your daily activities.
- Event recorder. An event recorder is a small device that you wear for several weeks or months. It records your heart’s electrical activity when you have symptoms of atrial fibrillation.
These tests can help your doctor to confirm the diagnosis of atrial fibrillation and to assess your risk of complications.
Treatment of atrial fibrillation
Treatment of atrial fibrillation (AFib) depends on the type of AFib you have, your symptoms, and your overall health. The goals of treatment are to:
Rate control vs. rhythm control
READ RELATED: Costco Members Share Tips on Choosing the Best Rotisserie Chicken
The two main approaches to treating atrial fibrillation are rate control and rhythm control.
Rate control aims to slow down the heart rate to a safe level. This can be done with medications called beta-blockers or calcium channel blockers. Rate control is often the first-line treatment for atrial fibrillation, especially in people with other medical conditions, such as heart failure or chronic kidney disease.
Rhythm control aims to restore and maintain a normal heart rhythm. This can be done with medications called antiarrhythmic drugs, cardioversion (an electrical procedure that resets the heart rhythm), or ablation (a procedure that destroys the tissue in the heart that is causing the abnormal rhythm). Rhythm control may be preferred for younger people with atrial fibrillation who have few other medical conditions.
Medications
There are a number of medications that can be used to treat atrial fibrillation. Some of the most common medications include:
- Beta-blockers: Beta-blockers slow down the heart rate by blocking the effects of the hormone adrenaline.
- Calcium channel blockers: Calcium channel blockers also slow down the heart rate by blocking the flow of calcium into the heart muscle.
- Antiarrhythmic drugs: Antiarrhythmic drugs work by restoring the normal electrical activity of the heart.
- Anticoagulants: Anticoagulants, such as warfarin and dabigatran, help to prevent blood clots from forming. Blood clots can cause strokes and other serious complications of atrial fibrillation.
Non-pharmacological treatments
There are also a number of non-pharmacological treatments that can be used to treat atrial fibrillation, such as:
- Lifestyle changes: Making lifestyle changes, such as losing weight, quitting smoking, and exercising regularly, can help to improve heart health and reduce the risk of complications from atrial fibrillation.
- Stress management: Stress can trigger atrial fibrillation. Learning to manage stress can help to reduce the frequency of episodes.
Procedures
If medications and lifestyle changes are not effective, your doctor may recommend a procedure to treat atrial fibrillation. Some of the most common procedures include:
- Cardioversion: Cardioversion is a procedure that uses an electrical shock to reset the heart rhythm. It is usually performed in the hospital.
- Ablation: Ablation is a procedure that destroys the tissue in the heart that is causing the abnormal rhythm. It is usually performed under general anesthesia.
The best treatment for atrial fibrillation depends on your individual circumstances. Your doctor will work with you to develop a treatment plan that is right for you.
How to reduce your risk of atrial fibrillation
There are a number of things you can do to reduce your risk of atrial fibrillation, including:
- Maintaining a healthy weight
- Eating a healthy diet
- Exercising regularly
- Managing other medical conditions, such as high blood pressure, heart disease, and diabetes
- Limiting alcohol consumption
- Don’t smoke
If you have any risk factors for atrial fibrillation, it is important to talk to your doctor about getting screened for the condition. Early detection and treatment can help reduce the risk of complications.
Complications of atrial fibrillation
Atrial fibrillation (AFib) is a heart condition that causes the upper chambers of the heart to beat irregularly. AFib can increase the risk of several serious complications, including:
- Stroke: AFib is the leading cause of stroke in adults. Blood clots can form in the atria of the heart in people with AFib, and these clots can travel to the brain and cause a stroke.
- Heart failure: AFib can weaken the heart muscle over time and lead to heart failure. Heart failure is a condition in which the heart cannot pump enough blood to meet the body’s needs.
- Other complications: AFib can also increase the risk of other complications, such as cognitive decline, dementia, and pulmonary embolism (a blood clot in the lung).
The risk of complications from AFib depends on a number of factors, including age, other medical conditions, and the type of AFib. However, even people with a low risk of complications should be treated for AFib to reduce their risk as much as possible.
Living with atrial fibrillation
Living with atrial fibrillation (AFib) can be challenging, but it is possible to live a long and healthy life with the condition. Here are some tips:
- Follow your doctor’s treatment plan carefully. This includes taking your medications as prescribed and making any recommended lifestyle changes.
- Monitor your symptoms. Pay attention to any changes in your heart rate, rhythm, or other symptoms, and report them to your doctor right away.
- Know your triggers. Some people with AFib find that certain things, such as stress, caffeine, or alcohol, can trigger episodes. Avoiding these triggers can help to reduce the frequency and severity of episodes.
- Get regular checkups. See your doctor regularly for checkups and monitoring. This will help your doctor to identify and treat any complications early on.
In addition to the above, here are some other tips for living with AFib:
- Eat a healthy diet. Eat plenty of fruits, vegetables, and whole grains. Limit saturated and trans fats, cholesterol, and sodium.
- Exercise regularly. Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
- Get enough sleep. Most adults need 7-8 hours of sleep per night.
- Manage stress. Find healthy ways to manage stress, such as exercise, yoga, or meditation.
- Quit smoking. Smoking can damage your heart and blood vessels and increase your risk of complications from AFib.
Living with AFib can be difficult at times, but with the right support and treatment, you can live a long and healthy life.
Monitoring your condition
Monitoring your condition is an important part of managing atrial fibrillation (AFib). It can help you to identify any changes in your symptoms or heart rhythm early on, so that you can seek treatment promptly.
There are a number of ways to monitor your AFib condition. Some of the most common methods include:
- Keeping a symptom diary. This can help you to track your symptoms over time and identify any patterns. You may want to note the date, time, and duration of each episode, as well as any other symptoms you experience, such as shortness of breath, dizziness, or chest pain.
- Using a wearable device. Wearable devices, such as smartwatches and fitness trackers, can be used to track your heart rate and rhythm. Some devices can also detect AFib episodes.
- Using a home monitoring device. Home monitoring devices, such as the KardiaMobile 6L, can be used to record an ECG (electrocardiogram) at home. This can be helpful for people who have occasional AFib episodes or who are at high risk for complications.
- Getting regular checkups. Regular checkups with your doctor are important for monitoring your AFib condition. Your doctor will listen to your heart and may perform an ECG to check your heart rhythm. They may also order blood tests to check for other medical conditions that could be contributing to your AFib.
If you notice any changes in your symptoms or heart rhythm, be sure to contact your doctor right away. Early detection and treatment of complications from AFib can help to improve your long-term prognosis.
Here are some additional tips for monitoring your AFib condition:
- Be aware of the symptoms of AFib. The most common symptom is palpitations, or a feeling of a racing or fluttering heart. Other symptoms can include shortness of breath, dizziness, lightheadedness, and chest pain.
- Keep a track of your heart rate and rhythm. This can be done with a wearable device, a home monitoring device, or by taking your pulse manually.
- Pay attention to your triggers. Some people with AFib find that certain things, such as stress, caffeine, or alcohol, can trigger episodes. Avoiding these triggers can help to reduce the frequency and severity of episodes.
- See your doctor regularly for checkups and monitoring. This will help your doctor to identify and treat any complications early on.




